Annually, more than 15 million people in Africa alone are pushed below the $1.90 a day poverty line, mainly attributable to household health expenditures1. More than 109 million Africans spend 10% or more of their household income on health2. Health is a human right, and equal access to affordable healthcare is key to ensuring that everyone benefits from this right. It is also economically advantageous for nations to have a healthier population, which translates to longer and more productive lives, higher income, and reduced healthcare costs.
The movement to accelerate Universal Health Coverage (UHC) is acknowledged as the solution towards a safer, healthier global population with respect to the human right to health. It encompasses access to quality health care services, vaccines and essential medicines, without suffering a financial burden.
To achieve UHC, countries would need to identify gaps and weaknesses in health systems and invest resources to strengthen them, and engage the public for beneficiary input.
Inadequate funding levels
In 2001, as per the Abuja Declaration, African governments met and pledged to allocate at least 15% of their annual budgets to the health sector. 3Global funders and donors also pledged to support the set up and roll-out of UHC in low and middle-income countries. Some countries, such as Rwanda and India have made considerable progress. In other countries, such as Kenya, the plans are underway towards a contributory government-led insurance-based health cover, with an ongoing dialogue involving the private sector and assessment of the public-private partnership sustainability. To date, several countries still need to make significant progress to meet the goals set by the Abuja Declaration. The health sector faces fierce competition for resources from other sectors, yet public health emergencies and non-communicable diseases (including neglected tropical diseases) are on the rise and global heath security challenges continue to confront the continent, placing demands for budget allocation to health. The situation is compounded by challenges of inefficiency in the deployment of resources and weak systems to ensure accountability and integrity at all levels of healthcare.
Donor funding played a major role to sustain healthcare services for many African countries since their independence. Successive governments had the delicate mission to find the right balance, and donor funding continues to run for most strategic public health programs such as immunization services, family planning, HIV/AIDS, Malaria and Tuberculosis. On the other hand, these countries are facing other financial burdens that leave them with little wiggle room to finance health and meet public expectations. Furthermore, these programs can benefit from better integration and coordination between the structures and systems that will contribute to them.
More challenges to overcome
Beyond these challenges on the journey to UHC, one study highlights 5 other barriers:
- Much of the population in Africa that live in extreme poverty and cannot afford any type of health insurance or healthcare expenses
- A large informal sector whose members are mostly uninsured
- A high dropout rate from insurance schemes
- Primary healthcare systems that suffer from insufficient funding
- A fragmented health insurance fund pool
For nearly two years, we have witnessed the ravaging effects of the COVID-19 pandemic across the world, forcing governments and external funding sources for Africa to shift their budgets towards tackling the immediate risks at home, boost intensive care and oxygen supply and ensure vaccines flow into the countries. African countries tried to keep the under-resourced health systems functional and responsive to the Covid-19 pandemic, mobilized local and external funds. With all these challenges and obstacles facing healthcare progress in the continent, will Africa achieve UHC by 2030?
Efficiency and innovations toward UHC
These challenges warrant exploration of new ways towards achieving UHC. Focused cost-minimization approaches need to be identified and embraced. African countries will need to look at efficient, innovative and evidence-based approaches and ensure that these reach the lowest levels of care, as discussed below:
- Strengthen the gate-keepers - With the roll-out of UHC, evidently more people will use the healthcare system. To ensure affordability of the health system, the primary healthcare facilities will have to function as gatekeepers to the next, more expensive levels of care. Therefore, it is required to strengthen lower level-primary healthcare facilities and win public confidence to make them their first point of call and entry into the health system. To win public confidence, the facilities need to stock adequate essential basic health care products, establish functional diagnostic services with consumables, deploy adequate human resources for health and have referral systems in place, backed by technology. Strengthening is needed at the low-level facilities to ensure they adopt business-like approaches with revenue plans and utilization targets, with trained management and leadership committees, which asks for capacity building.
- Ensure best utilization and deployment of technology - The accelerated use of technology is a major positive lesson from the COVID-19 pandemic; it brought efficiency and helped reduce costs in delivering health services, it generated data for decision-making and enabled appropriate deployment of interventions. Application of the right technology to support all health services can result in cost-minimization, increased efficiencies, and reduction of the administrative burden on human resources for health, to ensure more time is available for patientcare. Examples of areas to deploy technology are patient registration, electronic medical records, revenue collection and processing of billing and payments. In addition, departments like the pharmacy, laboratory and procurement may benefit from technology to ensure they stock accurate levels of commodities and reduce waste through expiries, detection of dead-stock, hoarding, deploy batch tracking and pharmacovigilance.
- Make evidence-based decisions - Efficiency and cost-minimization can only be reached if decisions are based on existing evidence. Therefore, it is key that governments have access to accurate information, so that they can analyze the context and implications, interpret and use it to their benefit in scaling up initiatives towards UHC in terms of health products and technology (including equipment and consumables for delivery of preventive and promotive services, diagnostic, curative and palliative/rehabilitative services.)
An example is the formation of a task force to ensure government market penetration in one of the East African Health Ministries. This task force is tasked to negotiate prices for various health commodities in the public sector. Conducting negotiations with a price reference based on existing data, like IQVIA’s sales audit, and having real-time insights in consumption and pricing across the country, will ensure they are able get the best deal.
Nationwide public health insurance schemes are possible, as the following case illustrates:
Case 1 – India
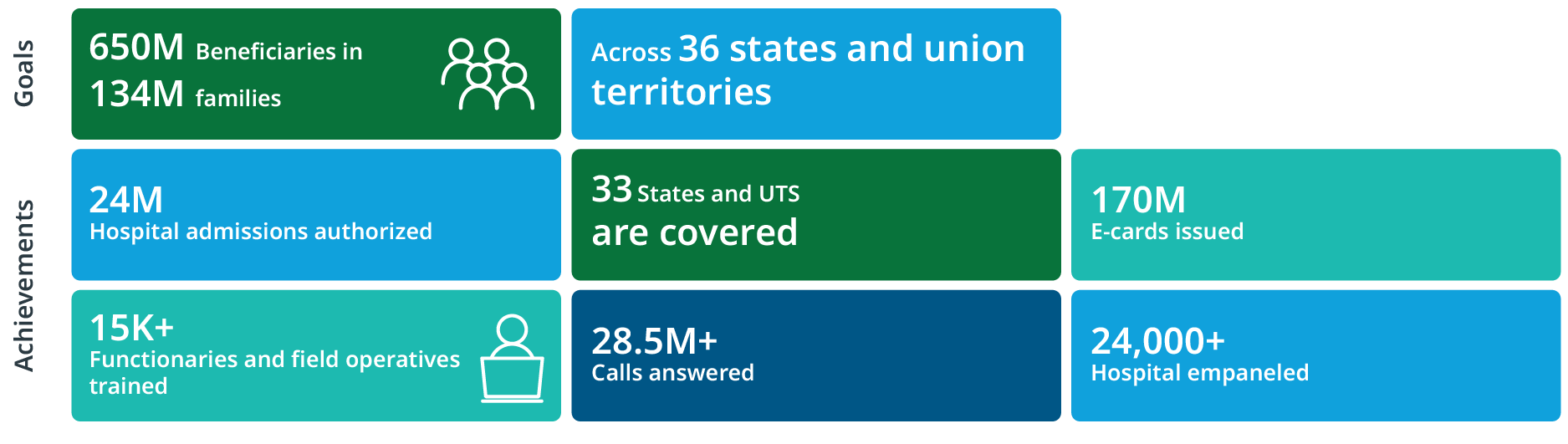
That the roll-out of a nationwide public health insurance scheme is feasible has been proven by India. Its UHC program, Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) aims to enrol 500 million beneficiaries that are currently at risk to fall into poverty due to health expenses.
Key pillars to a successful roll-out included:
- Ownership by the government through set-up of national health authority
- Inclusive enrollment of facilities in the scheme, public and private, primary and higher levels
- Roll-out of technology solutions like biometric identification, live fraud detection programs, etc.
- Continuous monitoring and evaluation to guide further implementation
Since the roll-out in 2018 the following has been achieved:
The IQVIA way
We believe that healthcare can be driven forward by improving efficiency, implementing innovations and using technology across the board. IQVIA supports governments to transform insights into intelligence, to make more confident and evidence-backed decisions that really make an impact. Decisions that help to get patients the right services of high quality that they deserve and still enjoy reasonable financial security. This is possible with unparalleled data, advanced analytics, transformative technology and domain expertise. IQVIA encourages countries to transform their healthcare insurance system using evidence as the base for each step as outlined below.
Case 2 – Evidence as base for UHC
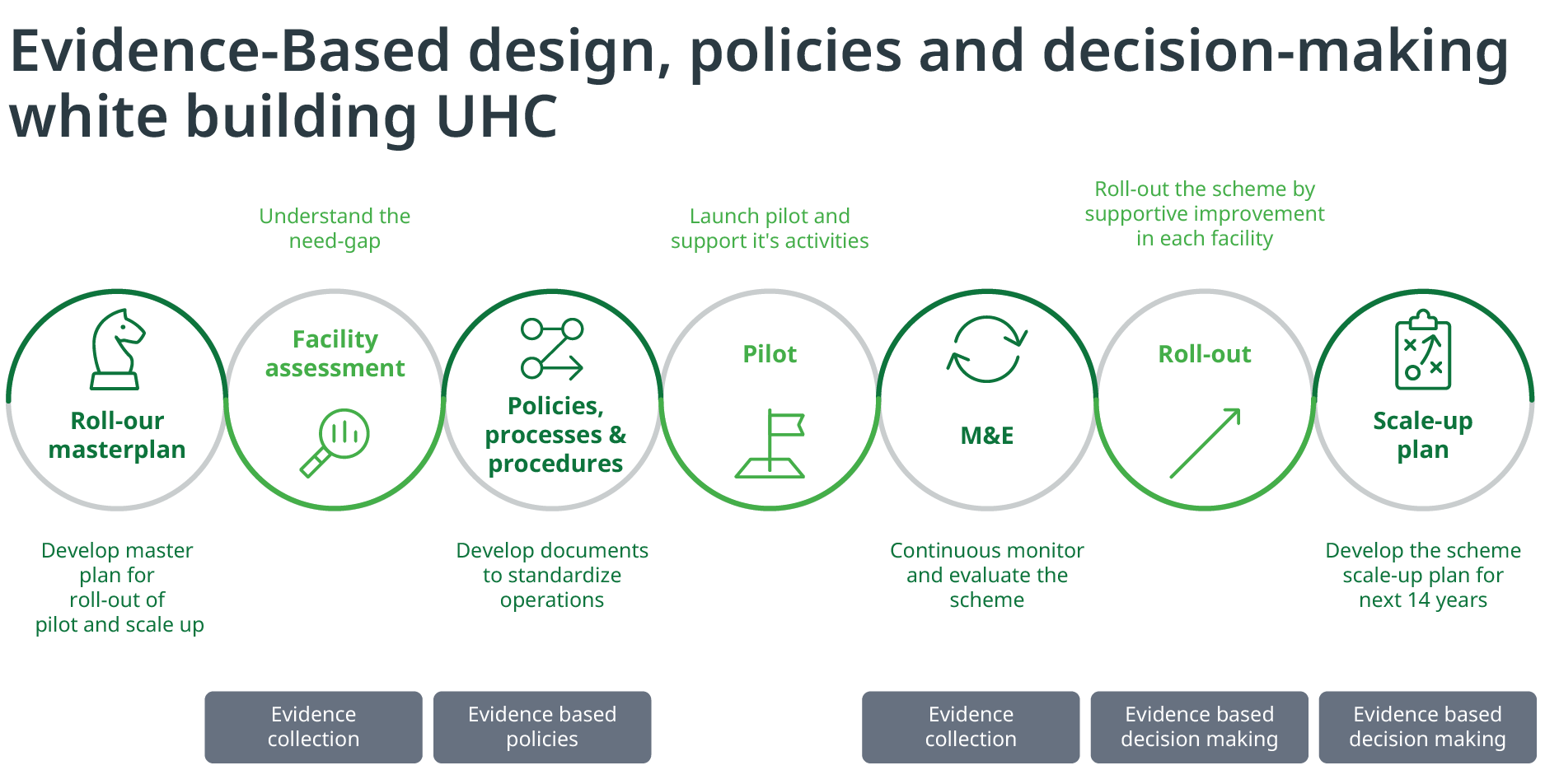
Working towards sustainable Universal Health Coverage invites new ways of doing business, with bold decisions based on evidence that can win public confidence into the future. At IQVIA we have the capability and solution offerings to support in making these decisions and rolling out the innovations, solutions and technologies that will make UHC to a success in your country.
IQVIA has a dedicated public-health focused practice actively engaged with governments, national/international donors, non-governmental organizations (NGOs) and private sector stakeholders to support evidence-based decision making. Our service offerings include Policy and Strategic Planning, Disease Burden Assessment, Research and Analytics including undertaking large community and institutional surveys, Monitoring and Evaluations of Large programs, Procurement and Supply Chain Assessments, Digital Health in Public Health, Public-Private-Partnerships, Support Private sector engagement and Program Implementation. The public health team serves more than 40 countries in the African, Middle East, and South Asian region. For more information, please reach out to Meshack Ndolo at meshack.ndolo@iqvia.com or Yvon de Jong at yvon.dejong@iqvia.com
1 https://www.who.int/data/gho/data/indicators/indicator-details/GHO/total-population-pushed-below-the-1.90-a-day-poverty-line-by-household-health-expenditures-(millions)
2 https://data.worldbank.org/indicator/SH.UHC.OOPC.10.TO
3 https://www.who.int/healthsystems/publications/abuja_report_aug_2011.pdf